
WELCOME TO THE WEB-SITE, INAUGURATED ON 30TH JUNE 2007 BY MR. MADHAB SAHA, MLA, TRIPURA LEGISLATIVE COUNCIL,FOR "HEPATITIS FOUNDATION OF TRIPURA",A SOCIETY REGD. UNDER THE SOCIETIES REGD. ACT OF 1860 NUMBERING 4065 AND ESTD. ON 28TH JULY 2002,AND THE PLATFORM OF COMMITTED CITIZENS OF TRIPURA STATEOF THE REPUBLIC OF INDIA,WORKING TOGETHER IN A UNIQUE BLEND OF UNITY TOWARDS A COMMON GOAL TO ENSURE PREVENTION & PROTECTION AGAINST HEPATITIS & OTHER DEADLY VIRUSES.
VIDEOs ON HEPATITIS & ABOUT ORG
Saturday, June 30, 2007
4TH ANNUAL TRIPURA STATE CONFERENCE 2007

ABOUT HFT:



HEPATITIS FOUNDATION OF TRIPURA
RAMNAGAR ROAD NO. 3 : AGARTALA - 799002
ABOUT US
THE ORGANISATION
Hepatitis Foundation of Tripura or HFT, an organization dedicated to work primarily in the field of liver disease & gradually, extending its zone of activities to many other health programs with the basic idea to develop mass awareness regarding health problem.
The organization was brought into the day light on 28th July, 2002 by the few members from different profession & position. The initial target was to arm people of Tripura with correct scientific knowledge about Hepatitis and Jaundice, so as to prevent unscrupulous practice of vaccination against Hepatitis B by the money mongers & Pseudo- social workers and to remove false believe and taboo about jaundice among common people.
THE BEGINING
The beginning days were not very smooth common believe that every so called “Social Organization” has got another face, also endangered our mere existence. The people and Govt. started weighing us in the same standard but we could prove ourselves and our vision, mission, & target and action became clear to everybody.
We started our activities from our temporary office at Teresa Diagnostic Centre, 7, Hospital Road, Agartala and HFT shall always remain thankful to this organization for initial boost.
Department of Health, Government of Tripura could be convinced about our mission and subsequently unscrupulous practice of vaccination against Hepatitis B was stopped. And eventually HFT has to shoulder the responsibility of Hepatitis B vaccination. From 15th December 2002 with the extreme help of journalist friends we could start our Hepatitis Clinic at Agartala Press Club for providing subsidizes Immunization against Hepatitis B to the people.
We launched our three point program i.e. :
A- wareness
I – mmunization
D – iagnosis, Counseling & treatment of Hepatitis B
On 6th March, 2003 the new Govt. took oath and Shri Tapan Chakrabory took over the charge of Department of Health, Govt. of Tripura. HFT was invited to explain the mission and vision of the organization. Hon’ble Minister after taking the stake of the situation adviced the members of HFT to dedicate for elimination of Hepatitis B from Tripura and extend and the activities of foundation to each every corner of the state.
Accordingly, the Deptt. of Health allowed HFT to run Hepatitis Clinic in Govt. Hospitals, utilizing MCH centre on every Sunday from 9 AM to 1 PM for Awareness, Immunization, Diagnosis and Treatment and Counseling.
The First official Hepatitis Clinic was inaugurated by Hon’ble Health Minister Shri Tapan Chakraborty on Doctor’s Day, i.e. 1st July, 2003 at Udaipur at T.S. Hospital, Udaipur and since then HFT members could never look back.
MEMBERSHIP
Any individual who pledges to our objectives and have a sense of Social responsibility and ready to work selflessly can be the member of Hepatitis Foundation of Tripura.
Our members, the “HFT FAMILY” is an unique blend of people from each and every strata of the Society including professionals like Doctors, Engineers, Businessmen, Govt. Officers, Govt. Employee, Nursing Staff paramedics, media personel, medical representatives, politicians, social activities, bankers, students and unemployed youth etc.
All are united for a common cause and this is definitely a rare “United forum” which is non-political & Non Government.
OUR MISSION
* To explain the preventive & protective aspect of various diseases in simplest manner to the people.
* Mass immunization against Hepatitis-B
* Expansion of activities by opening branches of the Foundation & Hepatitis Clinic
up to the peripheral level.
* To take active initiative for research on Hepatitis in Tripura
* To bring Hepatitis B vaccination under the preview of National Immunization
Programme
* To provide counseling services to the patient of Hepatitis and their relatives.
* Screening of family members of Hepatitis B.
* To provide necessary treatment to the patient of Hepatitis.
* To create a Hepatitis Registry in the state.
* To work in the field of HIV/AIDS to generate mass awareness, counseling, and
Prevention of Stigma.
* To participate in various Health related programme.
* To extend the activities in different sphere of health care delivery system.
OUR REGULAR PROGRAM.
1. Running of Hepatitis Clinic on every Sunday from 9 AM to 1 PM in all 26 branches (at present) for providing immunization, awareness and counseling and treatment services.
2. Organizing Awareness camps at length and breadth of the state.
3. Organizing Awareness program on HIV & AIDS.
4. Organizing awareness program in schools and colleges. (as permitted by the Department of School Education & Higher Education, Government of Tripura respectively).
5. Awareness campaign among TSR jawans, police and paramilitary forces.
6. Awareness campaign at Health Institutions among Health Care Providers.
7. Running Liver Clinic from 5 PM to 7 PM at the Central Office at Ramnagar Road No. 3, Agartala.
8. Regularly maintaining Central Office at Ramnagar Road No.3, Agartala, (Working hour 3 PM to 9 PM).
9. General & Specialist Health Camp at various places of state.
10. Publication of book, booklet, leaflet etc. for awareness.
11. Publication of Quarterly Newsletter from August 2006.
12. Observation of World Hepatitis Day on July 16th every year.
13. Organizing seminar on Hepatitis/Health related matters.
14. Organizing Super Specialist Health Camp for treatment of Hepatitis B & C / Other disease.
15. Awareness through print & electronic media.
16. Release of audio & video cassettes & CDs.
17. Organizing Quiz competition/Essay writing competition /sit & draw competition for students.
18. Participating in all Govt. program including “Health Fair” to propagate Health awareness.
19. Working with other professional & Health related organization.
20. Research activities in Hepatitis B & C and HIV & AIDS.
OUR FIELD OF ACTIVITIES
Though the HFT has started its activities as an organization to work for Hepatitis & liver disease but gradually our field of activates increased in many health related program. we were involved in :
i. Working in the field of Hepatitis Particularly for prevention of Hepatitis B & C.
ii. Immunization against Hepatitis B through out the state of Tripura at a highly subsidized rate. Present rate of vaccine is Rs. 20/- (rupees twenty) for children upto 10 yrs & Rs. 40/- (Rupees forty) for others.
iii. For diagnosis & treatment we are running “LIVER CLINIC” in our Central Office at Ramnagar Road No. 3, Agartala.
iv. Organizing Specialist Health Camp in various parts of the state.
v. Palliative care to the Cancer Patient.
vi. Program on AIDS.
vii. Anti tobacco program
viii. Awareness & early detection of cancer.
ix. Awareness of Member
x. Helping in NRHM program
xi. Awareness program on Diabetes and hypertension.
xii. Malaria related program
xiii. Research work on Hepatitis B & C and HIV / AIDS.
xiv. Geriatric Health Care Programs.
OUR ACHIEVEMENT
1. We have 26 branches through out the state & all 26 branches are working in a similar Tune.
2. We have Immunized _____ persons upto March 2008 ( Children : & Adult : )
3. Health Camp (upto March – 2008).
4. Super speciacilist Health Camp (Upto March – 2008).
5. Awareness Program
· Community Awareness program
· Institutional Awareness program
· Awareness program for Doctor
· Awareness program for Nursing Staff
· AIDS Awareness Programme
COMPLETED PROJECT
Palliative Cancer Care Project : and WHO sponsored the pilot project as per directive of Agartala Govt. Medical College.
ORGANIZATIONAL STRUCTURE
A two tier organizational system governs the total activities of the foundations.
Central Executive Committee (CEC) is the top most body to supervise all activities and all the branches are headed by the branch committee.
The CEC operates from State Capital Agartala and having its office at Ramnagar Road No. 3, Agartala.
It is maintaining liaison with all branches. CEC is a 15 Members Committee and Chairman & Secretary of all the branches are the members of this Committee by virtue of the post. It organizes meeting on every Sunday at 5 PM in the central office. Branch Committees are consisting of 11 members and organizes meeting on 1st Sunday of every month.
HEPATITIS CLINIC
Hepatitis Clinic are situated in MCH Centre of respective Govt. Health Institutions & provides Hepatitis B Immunizations at a subsides rate.
NET WORKING
STATE LEVEL
1. Net working Among the branches
2. Net working with All Tripura Govt. Doctors Association.
3. Net working with other Health Related Associations and Social Organizations.
4. Net workings with various democratic organizations.
NATIONAL LEVEL.
a) Liver Foundation, West Bengal
b) Hope initiative, Lucknow.
c) National Liver Foundation, Mumbai.
d) CMC, Vallore
e) AFTC
INTERNATIONAL LEVEL
a. BMS Foundation
b. CMMB.
CO-ORDINATION WITH VARIOUS GOVT. DEPTTS.
1. Deptt. Of Health , Govt. of Tripura.
2. Department of School Education, Govt. of Tripura.
3. Department of Higher Education Govt. of Tripura.
4. Department of Panchayat, Govt. of Tripura.
5. NSS
6. Tripura State AIDS Control Society
NEWS LETTER
HFT is publishing a quarterly bi-lingual News letter (English & Bengali) which is indexed with ISSN ( ISSN 0974-1097)
SOUVENIR
HFT is publishing a yearly scientific souvenir during the Annual Conference of every year named
“ HEPA CARE ”
ANNUAL CONFERENCE.
Every branch organizes Annual Conference in the month of April to June and the state conference is usually organized in the month of July & August.
REGISTRATION
We are registered society under Society Registration Act 1860 No. 4065-2002, of the Registrar of Society, Government of Tripura.
OUR ADDRESS
Central Office
RAMNAGAR ROAD NO. 3, AGARTALA, TRIPURA PIN - 799002.
PHONE NO. + 91 -0381 – 232-1166 FAX : + 91 -0381 – 232-1166


 OUR VISION:
OUR VISION:Y Hepatitis Free Tripura
____________________
OUR MISSION:
Y To generate mass awareness about Hepatitis in general and Hepat tis B & C in particular .
Y To explain the preventive & Protective aspect of the disease in siplest manner to all concerned.
Y Mass immunization against Hepatitis B.
Y Expansion of activities by opening Hepatitis Clinic up to the peipheral level.
Y To take active initiative for research on Hepatitis in Tripura.
Y To bring Hepatitis B vaccination under the perview of National immunization Programme.
Y To provide counseling services to the patient of Hepatitis and their relatives.
Y Screening of family members of Hepatitis B.
Y To provide necessary treatment to the patient of Hepatitis.
Y To create a Hepatitis Registry in the State.
Y To participate in various Health related programme.
Y To extend the activities in different sphere of Health Care delivery system.
___________
HEPATITIS FOUNDATION OF TRIPURA
____________
ABOUT US :
‘‘Never doubt that
a small group of committed citizens
can change the world
Indeed,that is the
only thing that ever has’’.
___ Margaret Meade
The Begining
__________
The Hepatitis Foudation of Tripura was born on 28th July 2002 with dedicated citizens of almost every profession such as doctor, engineer, businessman, media personnel, medical representatives, nursing staff, paramedical workers, medical laboratory personnel, health personnel, politicians, high officials, bankers, social workers, students & many others.The Hepatitis Foundation of Tripura was formed at the time when the medical fraternity in Tripura was unaware of gravity of the disease hepatitis specially B & C in the state. It was well known fact that hepatitis B & C are many many times contagious than much talked disease of civilization -HIV. While International & National NGOs, central & state governments, media, social organization, whole of medical fraternity & even WHO are actively involved in mass awareness programme for HIV /AIDS disease & spending million for the same cause, remain silent for silent killer disease hepatitis. At this juncture some greedy pharmaceutical companies along with some pseudo social workers, organizations start vaccination against hepatitis B at highest cost possible without any sort of briefing or counseling about the disease. These so-called social workers looted people of Tripura at the cost of their unawareness & unknown fear of the disease. There was no scientific criteria or protocol followed for health beneficiaries before immunization. The Health Department of State Government did not have any control over them. At this juncture ‘‘Hepatitis Foundation of Tripura’’ emerged.
Our Success Story
The begining days were not very smooth.Common belive that every so called ‘‘ Social Organisation’’ has got another face, also endangered our mere existence. The people & the govt. started weighing us in the same standard but soon we could proof ourselves and our vision, mission, target and action become clear to everybody. Our first success come in the form of ‘‘stopping’’-unscrupulous use of Hepatitis-B vaccine by money mangers. On 15 th December'02-our first Hepatitis Clinic started functioning at ‘‘Agartala Press Club’’ with the active support of Journalist friends. In March'o3 new Govt. took oath and new Heath Minister Shri Tapan Chakraborty gave us a patience hearing and Dept. of Health permited us to work in Govt. Hospitals by running Hepatitis Clinic on every Sunday using MCH centre of the Govt. Hospitals. The first offical ‘Hepatitis Clinic’ was inaugurated by Health Minister Shri Tapan Chakraborty at T.S. Hospital ,Udaipur on Doctor's Day i.e lst July'03 and on 6th July '03 Hepatitis Clinic of Agartala was shifed to IGM Hospital. On July 27th ‘03 Health Minister Shri Tapan Chakraborty inaugurated Hepatitis clinic at RGM Hospital, Kailasahar and Sub-Divisional Hospital, Dharmanagar. And since then people from every corner of state started requesting to open ‘Hepatitis Clinic’ in their respective Hospitals. Working hand in hand with Dept. of Health, Govt. of Tripura, Foundation started expanding its area of activity from one corner of state to other i.e kanchanpur to Sonamura to Sabroom. Today Foundation has branches 19 throughout the state but expansion program is continuously & corstantly progressing.
Our reach & awareness
Foundation members are working together in a unique blend of unity towards a common goal prevention & protection against hepatitis among those not affected by the disease & improving quality of life for all those affected by disease. We are gradually reaching out to the people of Tripura through our weekly (every Sunday) hepatitis clinic in all most all subdivisions in spite of some geographically difficult places. The members including doctors are providing the necessary help to the beneficiaries in the hepatitis clinics. The members conduct hepatitis awareness programme by giving health talk in health camps, community gatherings, health personnel worshops & meetings, school & college health awareness programmes, by distributing disease information leaflets in local languages, by banner writing, by permanent board writings in public places & health centers, through local cable network, by participating in health fairs, by conducting quiz competition & essay writing competition among school & college students, publishing informative articles in local languages in local daily, by health talks & discussion in TV, radio & many other ways. We get enormous support from electronic and print medias.
Our Tower of Strength
The source of inspiration and enthusiasm of every member of Hepatitis Foundation of Tripura through out the state is our Hon’ble Chief Minister Sri Manik Sarkar, who always spare his valuable time by his presence in our programme and by giving advice and guidance to our members as and when we are in need.
Our Friend, Philosopher and guide is our beloved Health Minister Sri Tapan Chakraborty. He who regularly & constantly enquires about our activities and performance and continuously asking us to remain honest and dedicated to the people of Tripura.
Each & every member of council of ministers the State of Tripura always remains abreast & informed about the functioning of the foundation and always helping the organisation by the continuous patronage.
Elected members of three tier panchayat of the state are continuously encouraging the foundation in each of every tiers starting from Zillasabhadhipati to member of Panchayat & Nagar Panchayat.
The help extended by the Commissioner of Health Shri S.K.Roy, IAS is examplary . Director of Health Services, Director of family welfare and Department of Health as a whole and health care providers of every nook & corner of State are the activist of our struggle against hepatitis.
Definitely every member of the Foundation are the corner stone of the organisation. But this is people of Tripura who are the real tower of the strength of the foundation.
Our Programs :
1. Development of Mass awareness throughout the state about Hepatitis.
2. Immunisation against Hepatitis B at a highly subsidised rate.
3. Counselling of Hepatitis Patient & their family members, free of cost.
4. Investigation of Hepatitis at a subsicbised rate from our empaseled lass throught state.
5. Advice & suggestion regarding treatment of Hepatitis, free of cost.
6. To help the patients to procure medicine
7. To organise General/Specialist Health Camp at different places of the state to reach to the people who are in need.
Our Activities :
_____________
1. Running ''Hepatitis Clinic'' on every Sunday from 9 am to 1 pm in all 21 branches (at present) for providing -
AID:-
(a) Awareness
(b) Immunisation
(c) Diagnesis Counselling Treatment advice against Hepatitis.
2. Organising awareness camp at interior places/Health centres.
3. Organising awareness camp at Schools & Colleges (as permitted by Dept. of Education, Govt. of Tripura).
4. Awareness campaign at Health Institutions among Health Care Providers.
5. Awareness campaign among TSR jawans & other police and paramillitary forces.
6. General & Specialist Health Camp at various places of state.
7. Publication of book, booklet, leaflet etc. for awareness.
8. Publication of bi-monthly Newsletter from Aug’06.
9. Observation of World Hepatitis Day on July 16th every year.
10. Organising seminar on hepatitis/ Health related matters.
11. Organising Super Specialist Health Camp for treatment of Hepatitis B & C. / Other diseases.
12. Awareness through print & electronic media.
13. Release of audio & video cassettes & CDs.
14. Organising Quiz competition/Eassy Writing competition/sit & draw competition for students & develop mass awareness.
15. Participating in all Govt. program including ''Health Fair'' to propagate Health awareness.
16. Working with other professional & Health related organ fisation.
Our Tasks in Future :
______________
Hepatitis Foundation of Tripura targeted 35 lacs population of tiny beautiful Tripura, inspite of many odds we will go ahead to meet our future plans.
Our future plans are -
1. Expansion of activities of hepatitis Foundation of Tripura in every corner of state.
2. Research works & Projects on Hepatitis in Tripura.
3. To include Immunisation against Hepatitis B under Universal Immunisation Program (UIP)Expanded program of Imunisation (EPI).
4. Inclusion of hepatitis control programme in National Health Policy.
5. To make compulsory immunization against hepatitis B for all health care providers before joining service, and professional education like Medical, Nursing, Paramedical etc.
6. To make compulsory immunization against hepatitis B for all children before joining schools.
7. Compulsory Screening of all pregnant mothers for hepatitiis B.
8. Preoperative screening for Hepatitis B.
9. A Hospital for Liver (Patients)diseases.
10. A Permanent office of Hepatitis Foundation of Tripura at Agartala.
Our Financial Suppot:
________________
As our foundation is a non-profit organization, we depend on the help of our well wishers. We get generous support from pharmaceutical companies, druggist & chemist, social workers, donors, businessmen, various corporate houses, Govt. undertakings, Industries, Doctors, Advertisers & Politicians to run our foundation's activities through out Tripura.
Our Organizational Structure :
______________________
Hepatitis foundation of Tripura is now becoming stronger & stronger with active cooperation of all members throughout the state. At present we are having 21 branches throughout the state and our target is very high and we strongly believe that by the end of 2007, presence of Hepatitis Foundation Of Tripura will be felt in every corner of the state.
All the branches are supervised by the 15 member Executive Comittee from its temporary office at Hotel Royal Guest House, Palace compound (West), Agartala.
Activities of every branch are supervised by 11 member branch comittee.
Annual Conference :
______________
Every branch organises Annual conference in the month of April & May. The state conference is being organised in the month of June or July every year. The III Annual Conference was organised on 16th July 2006 at Agartala & IV Annual congace at Udaipur an 30th June & 1st July 2007.
Our Souvenir :
__________
We publish yearly souvenir ''Hepa Care'' - during our state Annual Conference.
Our News Letter :
We have started publishing bimonthly News Letter from Aug'06 for free circulation.
OUR WEBSITE :
___________
http://www.hepatitisfoundationoftripura.blogspot.com/
Inaugurated of 30th june 2007 at 4th annual state conference held at Udaipur.
Membership :
__________
Any individual who pledges to our objects and have a sense of social responsibility and ready to work selflessly can be the member of Hepatitis Foundation of Tripura.
Communication :
____________
Hepatitis Foundation of Tripura
C/O : Hotel Royal Guest House,
Palace Compound (West),
Agartala - 799001, Tripura.
Ph :(+91) (0381) 2313781 - 84, 2321166
Fax :(91) 381-2324958
email : hft.cec@gmail.com
hepacare@yahoo.co.in.
HEPATITIS B VACCINE & INVENTOR:

PICTURE OF JENNER, INVENTOR OF FIRST VACCINE.
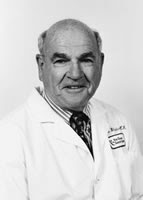
HEPATITIS B VACCINE INVENTOR:

Dr. Baruch Samuel Blumberg
BY
The research, discoveries and vision of Nobel laureate Baruch S. Blumberg, M.D., Ph.D., have had a far-reaching impact on public health around the globe. He has been responsible for major insights into the pathogenesis and prevention of hepatitis B infection-endemic in many populous nations, especially in Asia and Africa-and the fatal liver diseases associated with it. These include primary cancer of the liver, or primary hepatocellular carcinoma: one of the world’s three most deadly cancers, with death often occurring less than a year after diagnosis. Worldwide, primary liver cancer is the sixth most common cancer in men and the eleventh most common cancer in women. Blumberg identified the Hepatitis B virus, and later developed the diagnostic test and vaccine for it.
Dr. Blumberg was awarded Nobel Prize in 1976 in Physiology or Medicine. He shared the Nobel Prize with D. Carleton Gajdusek. The Nobel Prize was awarded for “discoveries concerning new mechanisms for the origin and dissemination of infectious diseases” and specifically, for the discovery of the hepatitis B virus.
In full Baruch Samuel Blumberg born in Brooklyn, New York, on July 28, 1925. Blumberg first attended Far Rockaway High School in the early 40s. He the attended Union College in Schenectady, NY and graduated in Physics with honors in 1945. He then entered the graduate program in mathematics at Columbia University but his interests turned to medicine and he enrolled at Columbia’s College of Physicians and Surgeons, from which he received his M.D. in 1951. He remained at Columbia Presbyterian Medical Center for the next four years, first as a resident and then as an intern.
As a medical student, he spent one summer at a mining company hospital in Surinam, South America, where he got his first taste of clinical research. Later, as an intern and assistant resident at New York City’s Bellevue Hospital, he experienced all the demands of patient care under crowded urban conditions. After a clinical fellowship at Columbia Presbyterian Medical Center, he went to England to earn his doctoral degree at Oxford’s Balliol College and earn his Ph.D. degree in biochemistry from Oxford University in 1957.
In 1957 he returned to the United States to join the National Institutes of Health and In 1960 he became chief of the Geographic Medicine and Genetics Section of the U.S. National Institutes for Health, in Maryland and hold this position until 1964. In 1964 he was appointed associate director for clinical research at the Institute for Cancer Research (later named the Fox Chase Cancer Center) in Philadelphia.
 In the early 1960s Blumberg was examining blood samples from widely diverse populations in an attempt to determine why the members of different ethnic and national groups vary widely in their responses and susceptibility to disease. In 1963 he discovered in the blood serum of an Australian aborigine an antigen that he later (1967) determined to be part of a virus that causes hepatitis B, the most severe form of hepatitis. The discovery of this so-called Australian antigen, which causes the body to produce antibody responses to the virus, made it possible to screen blood donors for possible hepatitis B transmission. Further research indicated that the body’s development of antibody against the Australian antigen was protective against further infection with the virus itself. In 1982 a safe and effective vaccine utilizing Australian antigen was made commercially available in the United States.
In the early 1960s Blumberg was examining blood samples from widely diverse populations in an attempt to determine why the members of different ethnic and national groups vary widely in their responses and susceptibility to disease. In 1963 he discovered in the blood serum of an Australian aborigine an antigen that he later (1967) determined to be part of a virus that causes hepatitis B, the most severe form of hepatitis. The discovery of this so-called Australian antigen, which causes the body to produce antibody responses to the virus, made it possible to screen blood donors for possible hepatitis B transmission. Further research indicated that the body’s development of antibody against the Australian antigen was protective against further infection with the virus itself. In 1982 a safe and effective vaccine utilizing Australian antigen was made commercially available in the United States.In 1977 he became professor of medicine, human genetics, and anthropology at the University of Pennsylvania. In 1989 he returned to Oxford to become master of Balliol College, a position that he held until 1994. Upon his return to the United States, he resumed his post at the Fox Chase Cancer Center, gaining the title Distinguished Scientist, and continued to teach as professor of medicine and anthropology at the University of Pennsylvania.
In 1993, he and his co-inventor, Dr. Irving Millman, were elected to the National Inventors Hall of Fame for their invention of the hepatitis B vaccine and the diagnostic test for hepatitis B. He has taught medical anthropology at the University of Pennsylvania and elsewhere, and has been a visiting professor in India (Bangalore), Singapore, University of Kentucky (Lexington), Indiana University (Bloomington), the University of Otago, Dunedin, New Zealand, and Stanford University.
In May 1999 Blumberg was appointed director of the National Aeronautics and Space Administration (NASA) Astrobiology Institute. He held several different positions while at NASA, where he remained until 2004.
(The writer is a member of Hepatitis Foundation of Tripura, Agartala)
MORE INFORMATION from NOBEL PRIZE website:
http://nobelprize.org/nobel_prizes/medicine/laureates/1976/blumberg-autobio.html
MORE INFORMATION :
B Jul 28 1925 Vaccine Against Viral Hepatitis and Process; Process of Viral Diagnosis and ReagentVaccine for Hepatitis BPatent Number(s) 3,636,191; 3,872,225Inducted 1993Baruch Blumberg discovered an antigen in 1963 that detected the presence of hepatitis B in blood samples. Hepatitis B is a potentially fatal disease often transmitted through blood transfusions. This hepatitis antigen, 'the Australia Antigen,' was found frequently in the blood serum of viral hepatitis sufferers. The antigen was named for an aborigine blood sample that reacted with an antibody in the serum of an American hemophilia patient. Working with Blumberg, microbiologist Irving Millman developed a test that identified hepatitis B in blood samples. The blood test screened out carriers of this infectious disease, and after blood banks began using the test in 1971, hepatitis B after blood transfusions decreased by 25 percent. Invention ImpactThe test also became the first method for screening blood donations for the hepatitis B virus. Together, Blumberg and Millman developed a vaccine against the virus. This vaccine protects people exposed to hepatitis B from infection and has been administered to millions, particularly in Asia and Africa. Since hepatitis B is an unknown factor associated with the development of liver cancer, the vaccine was the first against a major form of cancer. Inventor BioBorn in New York City, Baruch Blumberg graduated from Far Rockaway High School then joined the Navy, which assigned him to study physics at Union College in Schenectady, New York (B.S. 1946). He has an M.D., 1951, from Columbia University, and a Ph.D. in biochemistry, 1957, from Balliol College at Oxford University. He worked at the National Institutes of Health from 1957 to 1964 then joined Fox Chase Cancer Center and was also appointed professor of medicine and anthropology at the University of Pennsylvania. Blumberg shared the Nobel Prize in Medicine and Physiology in 1976. In 1989, he became Master of Balliol College at Oxford while maintaining a position at Fox Chase Cancer Center. Irving Millman was born in New York City. He received a B.S. in 1948 from City College in New York, an M.S. in 1951 from the University of Kentucky, and a Ph.D. in 1954 from the Northwestern University Medical School, where he was appointed assistant professor. He joined Fox in 1967 after having previously held positions with Armour & Company, the Public Health Research Institute of the City of New York Inc., and the Merck Institute for Therapeutic Research. He is an adjunct professor of biology at Hahnemann University in Philadelphia. He has been a member of the New York Academy of Sciences, the American Association for the Advancement of Science, and the American Society of Microbiology and is a fellow of the American Academy of Microbiology.
SOURCE : http://www.invent.org/hall_of_fame/17.html
_______________________
SOURCE : http://www.invent.org/hall_of_fame/103.html
HEPATITIS B :

PHOTO source: www.vaccineinformation.org/hepb/photos.asp
What causes hepatitis B?
Hepatitis B is a liver disease caused by the hepatitis B virus (HBV).
How does HBV spread?The spread of HBV occurs when blood from an HBV-infected person enters the body of a person who is not infected. This can occur through having sex with an HBV-infected person without using a condom (the efficacy of latex condoms in preventing infection with HBV is unknown, but their proper use may reduce spread of HBV).
Sex contact is the most common reason for the spread of HBV infection in the United States. The spread of HBV from male to female or female to male accounts for about 1 out of 3 acute (recently acquired) HBV infections in adults. The risk of spreading HBV increases if the male or female has multiple sex partners, a history of a sexually transmitted disease, or has sex with an HBV-infected person. About 1 out of 4 acute HBV infections occur among men who have sex with men.
 HBV is also easily spread by sharing drugs, needles, or "works" when "shooting" drugs. The risk of HBV infection from HBV-contaminated needlesticks is much greater than the risk of spreading HIV by this method. In the United States, illegal drug use injection accounts for about 16 out of 100 acute HBV infections. Other types of percutaneous (through the skin) exposures, including tattooing and body piercing, have also been reported to result in the spread of HBV when good infection control practices have not been used. Unsafe injections in medical settings are a major source of HBV spread in many developing countries and might be a risk for United States residents traveling abroad, if medical care is required in settings that have poor infection control practices.
HBV is also easily spread by sharing drugs, needles, or "works" when "shooting" drugs. The risk of HBV infection from HBV-contaminated needlesticks is much greater than the risk of spreading HIV by this method. In the United States, illegal drug use injection accounts for about 16 out of 100 acute HBV infections. Other types of percutaneous (through the skin) exposures, including tattooing and body piercing, have also been reported to result in the spread of HBV when good infection control practices have not been used. Unsafe injections in medical settings are a major source of HBV spread in many developing countries and might be a risk for United States residents traveling abroad, if medical care is required in settings that have poor infection control practices.HBV is also spread through needlesticks or sharps exposures on the job and from an infected mother to her baby during birth. Breastfeeding has not been associated with the spread of HBV.
HBV can also be spread during childhood. Most early childhood spread occurs in households of people with chronic (life-long) HBV infection, but the spread of HBV has also been seen in daycare centers and schools. The most likely way that the spread of HBV occurs during early childhood involves contact between an infected person's body fluids (e.g., their blood or drainage from their wounds or skin lesions) and breaks in the child's skin. HBV can be spread also when an HBV-infected person bites another person who is not infected. HBV can be spread also by an infected person pre-chewing food for babies, and through contact with HBV from sharing personal-care items, such as razors or toothbrushes. The virus remains infectious and capable of spreading infection for at least seven days outside the body. Virus can be found on objects, even in the absence of visible blood.
HBV is not spread through food or water, sharing eating utensils, hugging, kissing, coughing, and sneezing or by casual contact, such as in an office or factory setting. People with chronic HBV infection should not be excluded from work, school, play, childcare, or other settings.
How long does it take to show signs of illness after coming in close contact with a person who has HBV infection?
The incubation period ranges from 45 to 160 days (average 120.)
What are the signs and symptoms of hepatitis B?
About 7 out of 10 adults with acute hepatitis B have signs or symptoms when infected with HBV. Children under age 5 years who become infected rarely show any symptoms. Signs and symptoms of hepatitis B might include nausea, lack of appetite, tiredness, muscle, joint, or stomach pain, fever, diarrhea or vomiting, headache, dark urine, light-colored stools, and yellowing of the skin and whites of the eyes (jaundice). People who have such signs or symptoms generally feel quite ill and might need to be hospitalized. Every year, approximately 100-200 Americans die of fulminant (overwhelming acute infection) hepatitis B.
How serious is hepatitis B?
Hepatitis B is very serious. About 9 out of 10 infants (who do not receive appropriate prophylaxis at birth), 30 out of 100 children younger than age 5, and 2-6 out of 100 adults who are infected with HBV are unable to clear HBV from their bodies and become chronically infected. This serious condition is discussed below. Even though people might eventually recover from their acute infection, a feeling of tiredness and poor health might last for months.

What does it mean to have chronic HBV infection?
People with chronic HBV infection are infectious and can transmit HBV to others. Usually, chronically infected people do not feel sick and do not realize they are infected. They generally have HBV infection for their entire lives. They are also at high risk of developing chronic liver disease, including cirrhosis (scarring of the liver), liver failure, and liver cancer.
What are the complications of chronic HBV infection?An estimated 15-25 people out of 100 with chronic HBV infection eventually develop serious liver disease. Chronic HBV infection is responsible for most HBV-related sickness and death, including cirrhosis, liver failure, and liver cancer. When people are infected at a very young age, these forms of liver disease do not appear usually until young adulthood or middle age.
Is HBV infection a serious problem in the world?
In the United States, an estimated 3,000-4,000 people die each year of HBV-related cirrhosis, and another 1,000-1,500 die each year of HBV-related liver cancer. Worldwide, the medical consequences of chronic HBV infections are a huge problem. Approximately 350 million people around the world are chronically infected with HBV and approximately 1 million of these people die each year from cirrhosis leading to liver failure or liver cancer. The medical literature states that hepatitis B is the 10th leading cause of death worldwide.
What is the risk of getting HBV infection while traveling in other countries?
Short-term travelers to regions (Asia, Sub-Saharan Africa, Amazon Basin, Eastern Europe, and the Middle East) in which there are moderate to high rates of HBV infection are typically at risk for infection only through exposure to blood in medical, healthcare or disaster-relief activities; receipt of medical care that involves blood exposures; or sexual activity or drug use. The Centers for Disease Control and Prevention recommends hepatitis B vaccination for travel to any of these places, regardless of the length of stay.
How common is hepatitis B in the United States?
About 5 out of 100 people in the United States will contract HBV infection sometime in their lifetime, if not vaccinated. Approximately 0.8 to 1 million people have chronic HBV infection at the present time. Most of these people do not know they are infected.
During 1990-2005, the overall occurrence of reported cases of acute hepatitis B declined to a great extent. In 2005, the estimated number of new HBV infections was about 51,000--a decrease from an estimated 232,000 new infections in 1990. Racial and ethnic disparities for acute HBV infection were nearly eliminated for Asians/Pacific Islanders, American Indians/Alaska Natives, and Hispanics. However, in 2005, the occurrence of acute hepatitis B among blacks remained nearly three times higher than that among other racial/ethnic groups. In 2005, the highest occurrence of acute hepatitis B occurred among people ages 25-44 despite their race or ethnicity.
The overall decrease in the occurrence of acute hepatitis B in the United States is most likely due to the increased use of hepatitis B vaccine and changes in risk-reduction behaviors among at-risk populations in response to the HIV/AIDS epidemic. During 1990-2005, the greatest decline in cases was among children and adolescents, the group with the largest increase in hepatitis B vaccination coverage. Reporting of hepatitis B still remains a problem as many people do not exhibit symptoms recognized as hepatitis B and many cases/infections are missed and therefore not reported to health authorities.
Despite the dramatic decrease in the number of new HBV infections in the United States, chronic HBV infection remains a major problem. As stated above, about 1 million people have chronic HBV infection currently and most of these people do not know they are infected because they haven’t been tested. Most cases of chronic HBV infection in the U.S. are found in immigrants or refugees from areas of the world with moderate or high rates of hepatitis B. Some of these areas of the world include Asia, Africa, the Pacific Islands, and eastern Europe. People from these areas of the world should be tested to find out if they are chronically infected.
How does a person know if s/he has HBV infection?
A blood test called IgM anti-HBc is needed to diagnose acute hepatitis B. There are additional blood tests for hepatitis B that determine other aspects of HBV infection. These other blood tests can tell whether or not a person is currently infected and whether or not a person has been infected in the past. If the tests indicate a person has been infected in the past, testing will also determine whether the person has developed protective antibodies to the virus (i.e., they have gotten over the infection and will not get infected with HBV again [this is called immunity]) or whether they still have virus in their blood, indicating they might have chronic HBV infection.
What hepatitis B blood tests are available and what do they mean?
Hepatitis B surface antigen(HBsAg)
A positive test means that you have hepatitis B virus in your blood and can pass the virus to others. You could be recently infected or you could have chronic (life-long) infection. A negative test means that you do not have the virus in your blood.
Antibody to hepatitis B surface antigen(anti-HBs)
A positive test means that you are immune (cannot get hepatitis B). This positive test occurs when you were either vaccinated with hepatitis B vaccine successfully or you had the actual infection. Either way, this immunity means you will not get hepatitis B again.
Antibody to hepatitis B core antigen(total anti-HBc)
A positive test means you currently have or have had infection with hepatitis B virus at some undefined time period. The positive test has no relationship to having received hepatitis B vaccine; however, the test might be used prior to vaccination to see if you had already been infected.
IgM antibody subclass of anti-HBc(IgM anti-HBc)
A positive test means that you were recently (within 6 months) infected with hepatitis B virus.
Hepatitis B "e" antigen(HBeAg)
If this test is positive, you are infected with hepatitis B virus and have a large amount of hepatitis B virus in your blood. You are at increased risk of serious liver problems due to your chronic hepatitis B virus infection.
Antibody to hepatitis B "e" antigen(Anti-HBe)
This blood test might be positive if you have chronic hepatitis B virus infection or if you have already recovered from your infection. If have chronic hepatitis B virus infection and this test is positive, this means that you have low levels of hepatitis B virus circulating in your blood and are at lower risk of liver problems due to your chronic hepatitis B virus infection.
HBV Deoxyribonucleic acid(HBV-DNA)
When this test is positive, it means you are infectious to others and the hepatitis B virus is active in your body, possibly causing liver damage. The test is often used to determine success or failure of drug therapy if given for chronic hepatitis B virus infection.
Is there a medication to treat hepatitis B?There are several Food and Drug Administration (FDA)-approved medications that might help a person who has chronic HBV infection. These medications don't usually get rid of the virus, but they might decrease the chance of the infected person developing severe liver disease. Not everyone is a candidate for these medications. Researchers continue to seek additional cures for hepatitis B. There is no treatment (other than supportive care) for people with acute hepatitis B.
How long can a person with HBV infection spread HBV?
A person with acute or chronic HBV infection is contagious as long as they have the virus in their blood, which can only be determined by blood testing. In general, a person with acute hepatitis B gets rid of the virus in their blood in six months. If this does not happen, it is likely the person will become chronically infected with HBV for life.
What are some important Do's and Don'ts for people with chronic HBV infection?
DO's
Cover all cuts and open sores with a bandage.
Discard used items such as bandages and menstrual pads carefully so no one is accidentally exposed to your blood.
Wash hands well after touching your blood or infectious body fluids.
Clean up blood spills; then clean the area again with a bleach solution (one part household chlorine bleach to 10 parts of water).
Tell your sex partner(s) you have hepatitis B so they can be tested and vaccinated (if not already infected or vaccinated). Partners should have their blood tested 1-2 months after three doses of vaccine are completed to be sure the vaccine worked.
Use condoms (rubbers) during sex unless your sex partner has had hepatitis B or has been immunized and has had a blood test (as described above) demonstrating immunity to HBV infection. (Condoms might also protect you from other sexually transmitted diseases).
Tell household members to see their doctors for testing and vaccination for hepatitis B.
Tell your doctors that you are chronically infected with HBV.
See your doctor every 6-12 months to check your liver for abnormalities, including cancer.
If you are pregnant, tell your doctor that you have HBV infection. It is critical that your baby is started on hepatitis B shots within a few hours of birth.
DON'Ts
Don’t share chewing gum, toothbrushes, razors, washcloths, needles for ear or body piercing, or anything that might have come in contact with your blood or infectious body fluids.
Don’t pre-chew food for babies.
Don’t share syringes and needles.
Don’t donate blood, plasma, body organs, tissue, or sperm.
What should you do if you have been exposed to HBV?If you think you've been exposed to HBV, don't delay. Contact your doctor or clinic. If you have not been vaccinated, it is recommended that you receive treatment with hepatitis B immune globulin (HBIG). This is a blood product containing protective HBV antibodies. You should also get the first dose of hepatitis B vaccine as soon as possible, preferably at the same time as the HBIG is given, but at a different site on your body. Following this, you will need to complete the full hepatitis B vaccine series (usually a total of three doses over a six-month period).
Can you get hepatitis B more than once?No. If you get an acute case of hepatitis B and recover, you should have protective antibodies in your blood that will prevent any further infection with HBV. The medical literature does report possible mutant strains of HBV infection, but these are rare and would be highly unlikely to occur.
How does HBV differ from hepatitis A virus (HAV) and hepatitis C virus (HCV)?HBV, HCV, and HAV are viruses that attack and injure the liver, and can cause similar symptoms. Usually people get HAV infection from close personal contact with an infected person or from ingesting fecally-contaminated food or water. HBV and HCV are spread when an infected person's blood or blood contaminated body fluids enter another person's bloodstream. HBV and HCV infections can cause chronic liver problems. HAV does not. There are vaccines that will protect people from HAV infection and HBV infection. Currently, there is no vaccine to protect people from HCV infection. There are medications that are approved by the FDA for treatment of chronic HBV and HCV infections. If a person has had one type of viral hepatitis in the past, it is still possible to get the other types.
_____________
about vaccines
_____________
When did hepatitis B vaccine become available?
The first hepatitis B vaccine became commercially available in the United States in 1982. In 1986, a hepatitis B vaccine produced by recombinant DNA technology was licensed, and a second recombinant-type hepatitis B vaccine was licensed in 1989.
What are the names of the hepatitis B vaccines available in the United States?
The two recombinant vaccines (Recombivax HB® and Engerix-B®) are the only hepatitis B vaccine preparations currently used in the United States. (There are additional products licensed in the U.S. that contain these vaccines in combination with other vaccines.)
What kind of vaccines are they?The hepatitis B vaccines used in the United States are recombinant DNA vaccines, which means they are produced by inserting the gene for HBV into common baker's yeast where it is grown, harvested, and purified. HBV infection cannot occur from receiving hepatitis B vaccine.
How is this vaccine given?
Hepatitis B vaccine should be given to infants (12 months of age and younger) in the thigh muscle. Either the thigh or the upper arm muscle may be used for young children. The upper arm muscle is the preferred site of administration for adolescents and adults.
Who should get this vaccine?Hepatitis B vaccine, usually a three-dose series, is recommended for all children 0-18 years of age. It is recommended for infants beginning at birth in the hospital. All older children who did not get all the recommended doses of hepatitis B vaccine as an infant should complete their vaccine series as soon as possible. Most states require hepatitis B vaccine for school entry. Adolescents who are just starting their series will need two or three doses, depending on their age and the brand of vaccine used. Adults at increased risk of acquiring HBV infection should also be vaccinated. In addition, the vaccine can be given to any person who desires protection from hepatitis B.
What groups of adults are at increased risk of HBV infection?
Healthcare workers and public safety workers with reasonably anticipated risk for exposure to blood or blood-contaminated body fluids
Men who have sex with men
Sexually active people who are not in long-term, mutually monogamous relationships
People seeking evaluation or treatment for a sexually transmitted disease
Current or recent injection drug users
Inmates of long-term correctional facilities
People with end-stage kidney disease, including predialysis, hemodialysis, peritoneal dialysis, and home dialysis patients
Staff and residents of institutions or group homes for the developmentally challenged
Household members and sex partners of people with chronic HBV infection
Susceptible (non-infected) people from United States populations known to previously or currently have high rates of childhood HBV infection, including Alaska Natives, Pacific Islanders, and immigrants or refugees from countries with intermediate or high rates of chronic HBV infection. To see a list of these countries, go to http://www.cdc.gov/ncidod/diseases/hepatitis/b/country_listing.htm
International travelers to regions with high or intermediate rates of HBV infection. To see a list of these countries, go to http://www.cdc.gov/ncidod/diseases/hepatitis/b/country_listing.htm
In addition, any adult who wishes to be protected from HBV infection should be vaccinated without having to acknowledge a specific risk factor.
If you have not been fully vaccinated with hepatitis B vaccine and you are cared for in any of the following settings, you should ask the setting's healthcare provider to fully vaccinate you with hepatitis B vaccine. These setting include:
Sexually transmitted disease treatment facilities
HIV testing and treatment facilities
Facilities providing drug-abuse treatment and prevention services
Healthcare settings targeting services to injection drug users
Correctional facilities
Healthcare settings targeting services to men who have sex with men
Chronic-hemodialysis facilities and end-stage renal disease programs
Institutions and nonresidential day care facilities for developmentally challenged people
Who recommends this vaccine?The Centers for Disease Control and Prevention (CDC), the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), the American College of Physicians (ACP), and American College of Obstetricians and Gynecologists (ACOG) recommend this vaccine.
Is hepatitis B vaccine safe?Yes. Hepatitis B vaccines have been demonstrated to be safe when administered to infants, children, adolescents, and adults. Since 1982, more than an estimated 70 million adolescents and adults and more than 50 million infants and children have received at least one dose of hepatitis B vaccine in the United States. The majority of children who receive this vaccine have no side effects. Serious reactions are rare.
What side effects have been reported with this vaccine?
Of those children experiencing a side effect, most will have only a very mild reaction, such as soreness at the injection site (fewer than one out of three children) or low-grade fever. Adults are slightly more likely to experience such mild symptoms. Serious allergic reactions following hepatitis B vaccination are rare.
How effective is this vaccine?After three properly administered doses of vaccine, at least 9 out of 10 healthy young adults and more than 9 out of 10 infants, children, and adolescents develop protective antibodies and subsequent immunity to HBV infection.
Why is this vaccine recommended for all babies when most of them won't be exposed to HBV for many years, if then?
There are three basic reasons for recommending that all infants receive hepatitis B vaccine, starting at birth.
First, babies and young children have a very high risk for developing chronic HBV infection if they become infected at a young age.
It is estimated that about 1 out of 3 of the nearly 1 million Americans with chronic HBV infection acquired their infection as infants or young children. Those with chronic HBV infection are most likely to spread the infection to others. Infants and children who become chronically infected have an increased risk of dying prematurely from liver cancer or cirrhosis.
In contrast to other vaccine-preventable diseases of childhood, HBV infection in infants and young children usually produces no symptoms. Thus, the small number of reported cases of hepatitis B among children represents the tip of the iceberg of all HBV infections in children. For every child with symptoms of hepatitis B, there are at least 100 HBV-infected children with no symptoms---hence the increased risk to spread the infection to others without knowing it.
Second, early childhood infection occurs. About 16,000 children under 10 years of age were infected with HBV every year in the United States before routine infant hepatitis B vaccination was recommended. Although these infections represented few of all HBV infections in the United States, it is estimated that 18 out of 100 people with chronic HBV infection in the United States acquired their infection during early childhood. Clearly, infections occur among unvaccinated infants born to mothers who are not HBV-infected. In addition, unvaccinated foreign-born children account for a high proportion of infections. More effort needs to be placed on vaccinating these unprotected children.
Most early childhood spread of HBV occurs in households where a person has chronic HBV infection, but the spread of HBV has also been recognized in daycare centers and schools. The most probable ways children become infected with HBV are from skin puncture (e.g., biting) or from having their mucous membranes or cuts and scratches come in contact with infectious body fluids from an HBV-infected person. HBV remains infectious for at least seven days outside the body and can be found on and spread through sharing of inanimate objects such as washcloths or toothbrushes.
Third, long-term protection following infant vaccination is expected to last for decades and will ultimately protect against acquiring infection at any age.
Why should your child be protected against hepatitis B if h/she won't ever inject drugs or be sexually promiscuous?HBV can be transmitted in many ways in addition to sex contact and injection drug use. On average, an unvaccinated baby born in the United States has 5 out of 100 chances of developing HBV infection sometime during his or her lifetime. By avoiding obvious means of exposure, people can reduce their odds of becoming infected. But while there are degrees of risk involved in contracting HBV infection, there is no such thing as "no risk." Moreover, hepatitis B vaccine is the first vaccine to prevent cancer--HBV-related liver cancer.
Read "Unusual Cases of Hepatitis B Virus Transmission (Spread)" for examples of the spread of HBV in a variety of settings.
Will your child need a booster shot later in life?At the present time, booster doses are not recommended routinely for people with normal immune systems. Although the level of protective antibodies in the blood of a vaccinated person seems to decline with time, the immune system retains an immunization "memory" and if the person is exposed to HBV, the system "kicks in" and provides the needed protection.
Experts are continuing to monitor the long-term effectiveness of hepatitis B vaccine and will issue recommendations on the need for booster doses if evidence shows that booster doses are necessary.
Should I be tested before I get the vaccine to see if I'm already infected or immune?
Blood testing before vaccination is not recommended for the routine vaccination of infants, children, and adolescents. However, certain children, such as those born in countries where HBV is moderate or highly endemic (see the website above for a list of these countries), should be tested to be sure they are not already infected. Testing can be done at the same visit when the first dose of hepatitis B vaccine is given. Vaccinating a person already immune to or infected with HBV will not help or harm the person.
The main reason for testing people at increased risk for HBV is to determine if they are infected. If after testing they are found to be infected, they must be referred to a health professional for ongoing medical care for chronic HBV infection.
Should I get my blood tested after getting the vaccine series to make sure it worked?
Testing after vaccination is not recommended routinely. Testing after vaccination is recommended only for people whose medical care depends on knowledge of their response to the vaccine. This includes infants born to HBV-infected mothers; healthcare and public safety workers at risk of continued exposure to blood on the job; immune compromised people (e.g., people with AIDS or on hemodialysis); and sex and needle-sharing partners of people with chronic HBV infection. Testing should be performed 1-2 months after the last dose of vaccine.
What should be done if a person gets the first two doses of hepatitis B vaccine but never goes back for the final dose? Should the series be restarted?No, the series does not need to be restarted. If the series is interrupted after the first dose, the second dose should be given as soon as possible; the second and third doses should be separated by an interval of at least 8 weeks. If only the third dose is delayed, it should be administered as soon as possible.
The minimum recommended dosing intervals are 4 weeks between the first and second doses and 8 weeks between the second and third doses. The minimum interval between the first and third doses is 16 weeks.
Who should NOT receive hepatitis B vaccine?
People who had a serious allergic reaction to one dose of hepatitis B vaccine should not have another dose of hepatitis B vaccine. People with a history of hypersensitivity to yeast should not receive this vaccine. People with a moderate or severe acute illness should postpone receiving the vaccine until their condition is improved.
Can I get this vaccine when I am pregnant?
Yes.
I'm an adult who wants hepatitis B vaccination. How can I pay for the shots?
IN TRIPURA (INDIA) THERE IS NO SUCH POLICY, BUT ABROD , If you have insurance, the cost of hepatitis B vaccination might be covered. If not, these shots are often available at low cost through special programs or from health departments. Call your local health department for details.
Will hepatitis B vaccination protect me from hepatitis A or hepatitis C?
No.
Hepatitis A and hepatitis C are different diseases caused by different viruses. There is a vaccine for hepatitis A, but there is no vaccine for hepatitis C at this time.
________________
For information on hepatitis A and hepatitis C,
visit hepatitis clinics
run by
HEPATITIS FOUNDATION OF TRIPURA
CALL +91-0381-232-1166
MAIL US
OR
talk to your healthcare professional,
call your local health department,
AND ALSO
visit http://www.immunize.org/ and www.cdc.gov/hepatitis
THE TRIPURA MODEL:
 Hepatitis Foundation of Tripura
Hepatitis Foundation of TripuraPREVENTION OF HEPATITIS
THE TRIPURA MODEL
Tripura is small but beautiful. A healthy population is the index of state’s developmet & economy. Infective & communicable diseases disrupts the health of society. Hepatitis - or more specially Viral hepatitis is the cause of common disorder ''Jaundice'' - which causes loss of many man days.
Among various Viral Hepatitis - Hepatitis 'B' & 'C' may go into chronicity causing long - term sickness of liver. An unwell man unable to perform his activities - causing loss to him, his family, his society & state.
Chronic Hepatitis 'B' & 'C' remaining in persons body gradually destroys the liver and at the same time may cause liver cancer or liver cirrhosis.
Fortunately 'B' & 'C' - the two dangerous Hepatotrophic Virus can be Prevented by observing simple universal protective measure, like HIV/AIDS. Vaccine against Hepatitis 'C' is still in research laboratory but Hepatitis 'B' can easily be prevented by immunisation - a very effective and protective recombinant vaccine is in use through out the wold.
Hepatitis Foundation of Tripura spontaneously took the holy task of making Tripura Hepatitis free. It is a dream, a vision, a mission. But the scientific approach can convert the dream into reality.
Today our purview of discussion is hepatitis - 'B' and only this disease will be discussed subsequently. The outline of a model approach - ''The Tripura Model '' - is being presented in brief.
The Problem :
We do not have the exact figure of existing patients of hepatitis 'B' in Tripura but national figure is some where between 3 to 5% of population. If we consider the population of Tripura is about 35 lacs the burden is around 1.5 lacs (average) and this number will increase in a geometric proportion leading to many mortality, morbidity, loss of man days and destablizing state’s economy, which will be further jeopardized by highly expensive investigation and treatment of the patient.
The Target :
We are harbouring about 1.5 lacs of HepatitisB patients but we can not afford further increment of the number. So our target is; Not to allow anybody to get the virus of Hepatitis B de novo.
Is it possible ? Yes it is .
Hepatitis Foundation of Tripura is determined to achieve this goal.
The Project : The chronological approach :
Our approach to the problem starts from the mothers womb and let us draw the sketch of a man's life and the problem can be solved systemetically and chronologically.
1. Mothers womb :
It has been estimated that perinatal transmission or infection during childbirth is the commonest (40%) cause of transmission of Hepatitis B. All mother should routinely be tested for Hepatitis 'B' during ante - natal check up by simple & cost effective method of testing ''HBsAg''. All positive mother will be followed till confinement or child birth.
2. At Birth (Neonate) :
(a) Baby born to Hepatitis B positive mother will be given
i) Hepatitis B immunoglobulin injection at brith.
ii) Hepatitis B vaccine at brith and subsequently as per schedule. (0 - 1- 6 months)
b) Baby born to healthy mother will be given Hepatitis B vaccine at brith and
subsequently as per schedule.
3. 0 - 10 year of Age :
All children of 0 - 10 year should be immunised against Hepatitis B irrespective of caste, creed & sex, if not immunised earlier. This group is targeted as because - (1) Dose and cost of vaccine for this age group is less, (2) children are already following other immunisation schedule, (3) parents are more concerned about their children, (4) children are not aware of their problem.
4. 10 - 50 year of age :
Should ideally be immunised & vaccine is equally effective. This group of people are exposed to education, awareness programme through various media and can easily be convinced.
5. Above 50 years :
Effectivity of vaccine gradually decline with age but protection is always advocated.
6. Family Member of Hepatitis B positive patients :
Should by screened for HBsAG. Positive persons should undergo treatment and negative persons should immediately be vaccinated.
7. High Risk Group :
Health Care Providers : Doctors, Nurses, Paramedical workers, Laboratory technicians and other health workers should be immunised at the joining of their service and if not, later on at the first instance. Frequent blood receivers - Thallasemia and hemophilia patients, patient on hemodialysis, candidates for kidneys transplantation, candidates for major surgery, and cancer patients should receive immunisation at the earliest.
8. Don't give the disease to others :
If some one is harbouring the disease, please express - do no infect others.
9. health Care Providers please do not gift ''Hepatitis B'' virus to your patients :
Screen all patients for Hepatitis B (and C) before any surgical or invasive procedure.
10. Protect yourself :
Whenever receiving any injection please ensure sterility.Health care provider please do not get discase while treating patients.
Take only screened blood.
Is it so easy ? No, Never.
Education and awareness is the only key to success. Today even if an illiterate person receive any injury he immediately rushes for ''TOXOID'' injection. This has not happened in a day.
Today most of the parents are concerned about the routine immunisation of their children. This took decades to teach through global approach.
- Small pox is eradicated from the world.
- Polio is at the verge of eradication.
How ?
Through many years of teaching and awareness by WHO, World community, International NGOs, National & State Governments, Local NGOs, Text book teaching in educational institutions and medical fraternity.
What About Hepatitis B ?
v WHOs approach is hesitant.
v International NGOs are silent.
v National Government is indifferent.
v State Government is undone due to cost burden.
v No free vaccination against Hepatitis B, though all vaccine in Expanded
Programme of Immunisation (EPI) is free of cost.
v No commuity approach.
v Medical Fraternity is unaware of gravity of illness.
v Health Care Providers are also not immunised.
A Ray of Hope :
Many countries (about 116) has already included ''Hepatitis B'' in their national health programme. (not India). It stimulates others to take positive initiative.
A tough Task :
Definitely fighting all there odds is a very tough task but Hepatitis Foundation of Tripura's target is 35 lacs people of ''Beautiful Tripura'' - and with the help of ''You''this task is easy and the dream of'' Hepatitis Free Tripura'' will become reality.
Few - Suggestions :
1. Screen all pregnant mothers for Hepatitis B (and C)
2. Immunise all new born at brith. If missed, immunise today.
3. Inclusion of Hepatitis B in National Health Programme.
4. All Children upto 10 year of age should be immunised.
5. Family member of Hepatitis B patients should be screened for HBsAg and be immunised (if negative)
6. Pre-operative screening for HBsAg & compulsory immunisation against Hepatitis B before major surgery.
7. Use only screened Blood & Use only sterilized syringe.
8. Compulsory immunisation of Health care provider before joining service.
9. High Risk group - protect yourself.
10. Compulsory immunisation against Hepatitis B before admission in schools.
Hepatitis Foundation of Tripura's Programme :
1. Awareness generation throughout the State.
2. Counselling of patients and their family members.
3. Advice regarding treatment.
4. Immunisation at highly subsidised rate.
5. Expansion of programme to every corner of Tripura.
6. Scientific study in Tripura regarding prevalence and incidence of disease.
We know ..........
The task is tough.......... and miles to go before I sleep and miles to go before I sleep..
OUR GUIDELINE:
 HEPATITIS FOUNDATOIN OF TRIPURA
HEPATITIS FOUNDATOIN OF TRIPURAGuideline of Hepatitis B Vaccination
& Treatment
1. Definition
2. Epidemilogy of HBV
3. Risk groups and risk factors for HBV infection
4. Diagnosis and differential diagnosis
5. HBV vaccines and vaccination
6. HBV treatment
1. Definition
Hepatitis B is a viral diseases process caused by the Hepatitis B Virus (HBV). The virus is endemic worldwide. The virus is shed in all body fluids by individuals with acute or Chronic infection and by asymptomatic carriers, and is transmitted primarily by parenteral route such as blood transfusion or sharing needless. Oral transmission has a low efficiency. Sexual contact is a frequent cause. Healthcare workers are a high-risk group because of the risk of needlestick injury.
2. Epidemiology of Hepatitis B
Approximately 30% of the world’s population or about 2 billion people. have serological evidence of hepatitis B virus infection.
Of these, an estimated 400 million have chronic HBV infection and at least one million carriers die from liver cirrhosis and liver cancer each year.
The prevalence and incidence of HBV varies greatly in different areas of the world. The HBV virus is endemic worldwide with the areas of highest endemicity being China, Southeast Asia, sub-Saharan Africa, most Pacific Islands and the Amazon basin. In South America HBV is mstly not endemic. It is rare in children and more frequent in High Risk Groups.
In the developed world it is an illness affecting mostly high-risk adults, in the world’s poorer areas it is highly endemic and widely present in children. Any vaccination programmes in those areas therefore are best focused on immunization in infants and children whereas in the Western world it is better to focus vaccination on adults in high risk groups such as healthcare workers.
HBV infection leads to one of four outcomes :
a) Fulminant hepatitis
b) Recovery after acute infection
c) Chronic carrier state
d) Chronic Hepatitis B
The extent to which the outcome of HBV infections depends on immunological factors or on virus characteristics is uncertain. The age at which the infetion occurs plays a very important role. In infants under 1 yrs old, chronic infection will develop in 80-90% of cases, in children between 1-5 year 30-50% will go on to develop chornic infection. By comparison, 30-50% of adults who become infected HBV are symptomatic but only 2-6% of these adults develop chronic infection.
3. Risk groups and risk factors for HBV infection.
Adult Risk groups for HBV infection
Healthcare workers
Policemen
Migrant populations
Frequent travellers
Asylum seekers and refugees
Military personnel
Tourists
Students
Sex workers
Injecting drug users
Blood donors
Hemodialysis patients
Firemen
Hemophiliacs.
HBV tansmission routes :
HBV is transmitted through body fluids such as blood, semen, urine (Breast milk is controversial). The route can be :
Perinatal (From mother to baby at birth)
n From child to child
n From unsafe injections and transfusions.
n Unsterile instruments tatooneedles, dental equipments, other sharp objects.
n Sexual contact
n Unprotected sex (whether heterosexual or homosexual)
n Antibody of HBeAg (anti-HBe) indicating low infectivity and probably recovery
HBV is transmitted through either skin puncture or mucosal with blood or other infectious body fluids. The virus is found in highes concentrations in blood ans serous exudates.
Safe activities would include
Hugging
Shaking hands.
Preparing food
Swimming in a pool
There is no evidence of a possible link between HBV vaccination and multiple Sclerosis.
4. Diagnosis and differential diagnosis :
The Most common symptom of hepatitis infection is fatigue or tiredness. Fever, muscle and joint aches as well as nausea may also eccur. Some people will notice that their urine becomes darker and their skin will show a yellowish tint (Jaundice).
Principal symptoms
Fatigue and tiredness
Malaise
Fever
Muscle & Joint aches
Diacomfort in the abdomen on the right sise
Less common symptoms
Weight Loss
depression
Anxiety, Irritability
Headaches
Sleep disturbances
Itching
Appetite loss
HBV is one of 6 viruses know to cause hepatitis in humans and the acute clinical illness caused by there viruses maybe similar, Specific diagnostic tests are required therefore to determine the cause in each case. Differential diagnosis include CMV, EB virus and Herpes virus.
Serological tests are available commercially for a veriety of antigens and antibodies associated with HBV infection. HBeAG negative mutants are important subset of patients.
For antigens :
Hepatitis B Surface (HBsAg) for the presnse of the vireus.
Hepatitis B e antigen (HBeAg) correlates with viral replication and infectivity
For antibodies :
Antibody to HBsAg (anti-HBs)
Antibody to hepatitis B core antigen (anti-HBc) these antibodies to the core can be either IgM (acute) or IgG (chronic)
Other markers would be:
HBV DNA= indicates virus presence
DNA polymerase= determines the presence of HBV DNA
HBsAg in liver cells= Orcein stain=Shakata= HBsAg inside hepatocytes
Serological markers of HBV infection very depending on whether the infection is acute or chronic.
A diagnosis of acute HBV infection can be made on the basis of the detection of IgM class antibody to hepatitis B core antigen (IgM anti HBc) in serum; IgM anti HBc is generally detectable at the time of clinical onset and declines to subdetectable levels within 6 months. IgG anti-Hbc persists indefinitely as one progress to chronic infection. Anti HBs becomes detectable in patients who do not progress to chronic infection. The presence of anti-HBs after actute infection generally indicates recovery and immunity from reinfection.
In patients with chronic HBV infection, both HBsAg and IgG anti-HBc remain persistently detectable, generally for life. In addition, a negative test for IgM anti HBc together with a positive test for HBsAg in a serum specimen usually indicates that an individual has chronic HBV infection.
5. HBV vaccines and vaccination :
Introduction :
Since the discovery of HBV 25 years ago vaccination continues to be the best way for dealing with the condition, Hepatitis B is preventive and universal vaccination is probably best.
Two types of Hepatitis B vaccine are available :
Recombinant to genetically engineered vaccines are made using HBsAg. synthesized in yeast (Saccharomyces cervisiase) or in a mammalian cells into which the HBsAg gene has been inserted. Both consist of a suspension of HB sufrace antigen. Each country has different preparations.
Human plasma-Dervided Vaccines (PDV) are prepared from purified HBsAg from the plasma of persons with chronic HBV infection. There are more than 15 different PDVs licensed worldwide (not being used in India).
There are no significant differences in safety, immunogenicity or efficacy between these two types of vaccines.
HBV vaccines will generate protective (>10 IU/ML) Levels of antibodies to HBsAg in 95% of children and 90% of adults. Re-vaccination works in 30-50% of persons who did not respond to primary vaccination. Revaccination of non-responders is not recommended after two series of vaccination (6 doses).
A distinction can be made between Pre-Exposure and post-Exposure Vaccination.
Pre-Exposure Vaccination: In a country like India all children upto 10 years of age should be the target group.
However vaccination can be made at any age, High risk groups like Health Care providers, Family member of positive case, frequently blood transfusion receivers shall be vaccinated at the earliest Recombinant vaccine: (Any recombinant vaccine can be interchanged).
Child<10yr>10 yr 20 ug (1 Ml)
Adult 20 ug (1 ml)
Immunosuppressed person 40 ug (2 ml)
Dialysis person 40 ug (2 ml)
Post-exposure Vaccination :
A combination of Hepatitis B immunoglobulin (HBlG–‘‘Hepabig’’) vaccine is recommended.This is of especial relevance in neonates where an immediate start of post exposure immunisation will prevent neonatal infections of HBV infected mothers, It is important to vaccinate within 24 hours. There is no evidence of a protective effect if the vaccine is given after 7 days (0.5 mg)
Direct exposure (Percutaneous inoculation or transmucosal exposure) to HBsAg positive body fluid (eg Needle Stick Injury) :
HBlG single intramuscular dose of 0.06 mg/kg (as soon as possible).
Followed by complete course of HBV vaccination (within 7 days)
Direct Exposure following sexual contact with a patient with HBV
HBlg single intramuscular dose of 0.06 mg/kg (within 14 days)
Followed by complete course of HBV vaccination
Contraindications & Sideeffects :
There are very few contraindications
i) Servere allergic reaction to previous doses
ii) Severe allergic reaction to baker’s yeast (as used in making bread), plasma derived HBV vaccine can be used instead.
Fever> 38.50C
The following are not contraindications to administering HBV vaccine :
i) Any minor illness such as respiratory tract infection or diarrhea with a temperature below 38.50C,
ii) Allergy or asthma,
iii) Treatment with antibiotics,
iv) HIV Infection, more informatin is, however, needed on the efficacy of HBV vaccination in neonates or infants that are infected with HIV.
v) Breastfeeding
vi) History of seizures.
vii) Chronic illnesses
viii) Stable neurological conditions
ix) Prematurity or low birthweiht
x) History of jaundice at birth
xi) Pregnancy
Vaccination dosage Schedule :
Vaccination in infants, adolescents and adults involves a multistep process with the first two injections given one month apart and the 3rd one 6 months leter. (O - I - 6 months).
Drop out: It is to be emphasize that the person receives vaccines in time, however, in case of any delay for second dose it is to be observed that a gap of 4 months is maintained between 2nd and 3rd dose. and in case of 3rd does delay of one month may be allowed. It means a delay of one month can be allowed in either case. In case of further delay re-scheduling of three doses is to be done.
Immunogenecity is 95% in immuocompetent adults but can be reduced be age. It is 85% in those over 40 yrs and 75% in theose over 60 yrs of age. Vaccination in immunosuppressed patients is less effective.
For example in patients with:
n HIV
n Chemotherapy
n Steriod use
n Diabetes
n Chronic renal disease
n cirrhosis
n smoking
n obesitay
Vaccination Route & Site
Infants: intramuscular injection in the anterolateral aspect of the thigh
Older children : intramusccular injection in the deltoid muscle.
Adults : intramusccular injection in the deltoid muscle.
Injection equipment :
0.5 ml, 1.0 or > 2.0 ml syringe
25 mm, 22 or 23 guage needle
Vaccine Safefy & quality
Thermostabily
HBV vaccines should never be frozen. The frezing point of HBV vaccine is 0.50C
HBV vaccine is stable for at least 4 years if stored between 2-80C
HBV vaccines are relatively heat stable and have only a small loss of potency when stored for 2-6 months at a temperature of 370C
The Shake Test
It you see HBV vaccine Frozen then it is damaged. However, a vaccine may also have been frozen earlier and then thawed again. The Shake test can be used to check if the vacure has been damaged by earlier freezing.
n Compare the vaccine that you suspect has been frozen and thawed with vaccine from the same manufacturer that you are sure was never frozen.
n Shake the caccine vials
n Look at the contents carefully
n Leave the vaccines to stand side by side for 15-30 minutes for any sediment to settle
n Do not use it if a sediment settles below an almont-clear liquid.
6. HBV treatment
1. Treatment of acute HBV infection
A spontaneous recovery after acute infection with HBV occurs in 99% of previous healthy adults. Antiviral therapy is not likely therefore to improve the rate of recovery and is not required.
In fulfilment hepatitis meticulous intensive care may improve surviaval. Orthrotropic liver transplantation is the only proven therapy that improves patient outcomes.
2. Treatment of chronic HBV infection
Treatment of chronic HBV infection is difficult and limited in long-term efficacy.
There are three treatment options.
a) Interferon monotherapy
b) Lamivudine or other nuceloside anologue (Adfovir, Teloiyudine, entecavir)
c) Combination therapies of interfeorn with a nucledside analogue
A decision to treat must be based on a combination of
n Serum liver tests (increased serum AST and ALT levels)
n Virologic assays (presence of HVeAg or HBV DNA levels > 105 Copies/ ml
n liver histology (disease activity; fibrosis)
n Virologic tests to exclude HCV, HDV, HIV
If the disease is inactive or mild it is best to do nothing and to monitor ALT levels.
It the disease is moderate to severe, treatment must be recommended.
Initial Approch :
If a at HSsAg positive patient comes to you he should be clinically evacuated and should be observed weather he is having any sign and symptom of chronic liver disease.
Lab Diagnosis :
HBV patient should be admited for SGOT/SGPT and HBeAg and HBV DNA (quasition test) for make-up decision wheather he should be treated on not. Once liver function tests should be performed according to the clinical preservators to the patient.
decision to Treat :
When not to treat :
If a person is HBSeAg positive but ACT (SGPT) is normal and HBeAg is nagetive he should be considerd as inactive HBV infaction (or so called carrier) and should not be treated. But he should be evaluated at 6 monthly interval for stain of ACT.
When to treat :
i) If a human is HBsAg positive, ACT > 2 tinen of uper limit of normal, HBsAg is positive and / or HBV DNA is > 105 copies / ml.
ii) If a person is HBsAg positive ACT raines, HBeAg nagetive, but HBV DNA is > 105 copies / ml and / or an liver Biopcy avidence of fibrosis is injelartive (chronic hepatitis is remain).
What drug to be used :
i) Interferon is still best mode of treatment.
ii) Alternatively, Lamivudine, Telbivudine as entacavir and newer drug can be used.
iii) Combination of both the group of drug are used in mutant cases.
iv) In HBeAg nagetive, HBV DNA positive comes, interferon is only treatment.
v) The patient who are HBsAg positive, very high ACT and HBeAg positive comes oral medicines are effective.
vi) In decampesantal liver diseases, interferon should not be used.
* Inteferon-a-therapy recommended dose :
-5 Million Units (MU) daily or 10 Mu 3 times weekly
* 6 MU/m2 3 times weekly for children, subcutaneously, for 16 weeks (up to 32 weeks may be beneficial)
Advantages
* Short treatment duration
* No avtiviral resistance (but precore mutants might be induced by previous interferon treatment)
* Excellent duration and quality of response
Disadvantages
* Expensive
* Side-effects (interferon treatment may be associated with flares-sometimes severe flares)
* Parentaral route less efficacy
* Decompensated liver disease
Contraindications
psychiatric ilness, in particular depression and sucidal tendency
authoimmune or systemic disease
severe leukopenia or thrombocytopenia
Pequlated Interferon :
New forms of interferon are being developed in which the agent is covelently bound to polythylene glycon (PEG). The interferon is slowly relaesed as these covalent bonds degrade. PEGylated forms of interferon offer some advantage in case of use. They can be administered once a week only and they better meet the need for continous circulating levels of interferon.
Lamivudine therapy :
Long-term therapy with lamivudine is recommended for patients with advanced or decompensated chronic hepatitis B. Transplanation may become necessary because of deterioration in liver function, development of resistance of apearance of Hepatocillular carcinoma (HCC).
Recommended dose:
100 mg daily/oral
150 mg twice daily in HIV infected patients (and only in combination with other antiretrovirals)
Advantages
Easy to administrater and monitor
Few side-effects
Better response in selected groups (> 30% eAg loss)
Effective in subpopulation not responsive to Interferon.
Disadvantages
Long-term durability of response not as for interferon-alpha
Therapy often needs to be long-term (> 12 months)
Dose not produce HBsAg loss
Conclusion :
Treatment of hepatitis B is fill developing and in future, less expensive oral therapy of shorter duration may be available.

